Osteochondrosis is a chronic recurrent disease that occurs against the background of constant destruction of vertebrae and intervertebral discs.Depending on the localization of vertebrates undergoing degenerative changes, they distinguish between breast, lumbosacralis pathology, as well as the neck.The leading symptoms of osteochondrosis are pain, the severity of which increases during physical exertion, stiffness of movements.In the clinical picture, there are often vertebral signs: headaches, jumps in blood pressure, a decrease in visual acuity and hearing.
The diagnosis is based on the results of instrumental research - radiography, MRI, CT.In therapy of osteochondrosis, drugs of various clinical and pharmacological groups are used.To increase their clinical efficiency, physiotherapeutic and massage procedures are carried out.One of the main methods of therapy and prevention is physiotherapy exercises.
The mechanism of development of the disease
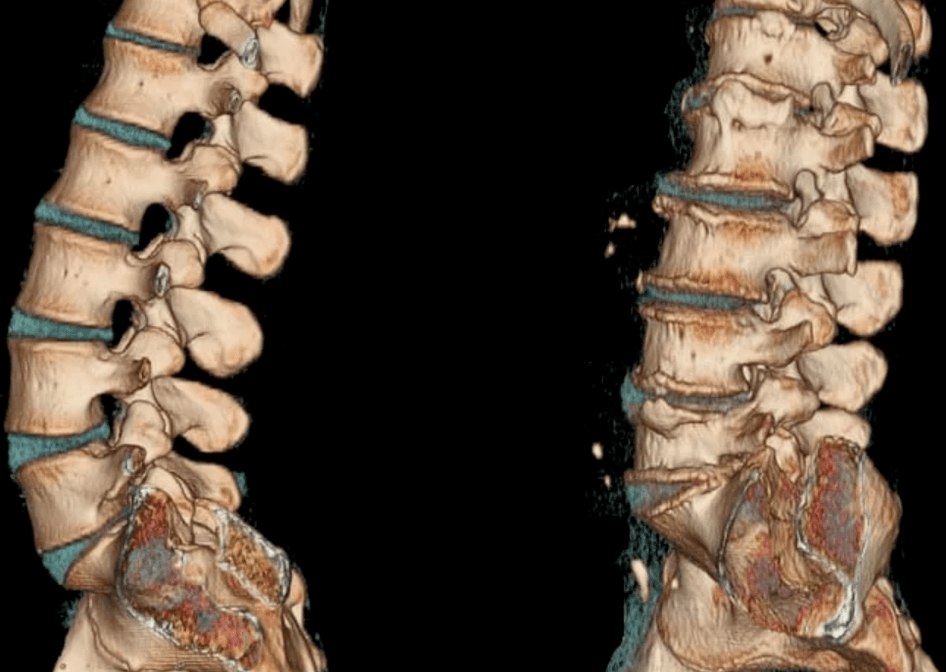
The pathogenesis of osteochondrosis is based on the loss of Pulposus by the core of its hydrophilic properties.This semi -liquid structure consists of connective tissue fibers and jacket.As a person grows up, there is a decrease in the vascular channel in each disk between the vertebrae.The intake of nutrients in it occurs diffusely, that is, according to the principle of spontaneous leveling of concentrations.This explains the impossibility of complete restoration of cartilaginous tissues after injury or excessive physical exertion on the spinal column.
The processes of osteochondrosis aggravate changes in the hormonal background and an unbalanced diet.The amount of nutrients sufficient for their full functioning does not enter the cartilage tissue, which provokes the following disorders of their structure and properties:
- strength and elasticity are lost;
- The form, consistency and configuration change.
Intervertebral discs are flattened, and radial cracks are formed in fibrous rings.This causes a reduction in the distance between neighboring vertebrae.Gradually, the connective tissues of fibrous rings and ligaments are involved in the pathological process.In response to the decay of tissues, the immune system begins to produce immunoglobulins, which leads to aseptic inflammation and the formation of edema in the joint of the joints and the soft tissues located nearby.The capsules of the joints are stretched, so the intervertebral discs cease to reliably fix the vertebrae.And with the instability of intervertebral segments, the likelihood of infringement of the nerve root or squeezing of the blood vessel increases.This often occurs with cervical osteochondrosis and causes its pronounced symptoms.
Causes and provoking factors
On the state of the intervertebral discs, the reduced tone of the skeletal muscles of the spinal column adversely affects.Irrational, asymmetric functioning of the muscles occurs with prolonged person in a non -physiological position, for example, with a head lowered while working at the computer.The destruction of cartilaginous fabrics can be provoked by the constant wearing of a heavy bag on one shoulder, a dream on a soft mattress and a high pillow.
The following external and internal negative factors also accelerate the destruction of the intervertebral discs:
- endocrine and metabolic disorders;
- infectious pathologies, especially chronic;
- preceding spinal injuries (compression fractures, bruises);
- frequent hypothermia;
- The presence of systemic or degenerative-dystrophic diseases-gouty, psoriatic, rheumatoid arthritis, osteoarthritis, osteoporosis.
If a person has bad habits, then he is at risk.Smoking and abuse of alcohol worsen the state of blood vessels, lead to insufficient blood circulation and to the deficiency of nutrients in the cartilage tissues of the disks.
In the presence of flat feet or clubfoot, the risk of developing osteochondrosis of any localization increases significantly.Such congenital or acquired defects become the reason for increasing the load on the spine due to the impossibility of ensuring proper depreciation with the support.The factor predisposing to the emergence of pathology is obesity.
With the deposition of adipose tissues in various parts of the body, support for equilibrium is complicated, which leads to the effects of excessive loads on the intervertebral joints.
Clinical picture
The first clinical manifestation of cervical, chest or lumbar osteochondrosis is back pain.During relapses, it is permeating, radiating to the nearby part of the body.The slightest movement leads to an increase in the severity of the pain syndrome.A person’s response is the adoption of a forced position in which the intensity of uncomfortable sensations is minimal:
- People with cervical osteochondrosis prefer to turn aside not their heads, but the entire body;
- With a breast pathology, a person is even afraid to take a full breath, as this becomes the cause of acute pain in the thoracic region;
- Patients with lumbar osteochondrosis are difficult to sit down, get up and go due to infringement of the spinal nerve.
Most patients complain to the doctor about stupid constant pains and a sense of constraining movements in the morning.This requires additional differential diagnosis to exclude myositis (inflammatory process in the skeletal muscles of the back) and osteoarthritis.The reason for the appearance of aching, pressing pains is the compensatory stress of muscle tissue to stabilize the affected vertebral-motor segment.The constant pain syndrome of weak or medium severity also occurs due to a significant stretch of the intervertebral disc and the development of aseptic inflammation.
For osteochondrosis of a certain localization, specific symptoms are characteristic.For example, with lumbar pathology, lumboyshialgia often occurs - a pain attack in the lower back and back of the thigh.Thoracic osteochondrosis is clinically manifested by visceral pains in the cardiac region, the right hypochondrium, stomach, numbness, increased skin sensitivity, crunch in the vertebrae.But the most pronounced and diverse symptoms are distinguished by a pathology that affects the cervical intervertebral discs.
As a result of the displacement of the vertebrae, the formation of osteophytes, the vertebral artery is compressed, which feeds the cells of the brain, which provides them with oxygen.A person suffers from violation of coordination of movements, noise in the ears, headaches, arterial hypertension.
What can be in the absence of treatment
Most complications of osteochondrosis occur due to the formation of hernia of the intervertebral disc.It is formed when this vertebral structure is displaced, which leads to a rupture of the posterior longitudinal ligament.The disk becomes even more unstable, and part of it protrudes into the cerebrospinal canal.A hernia is considered an exploding if, in the process of its formation, along with the disk, its Purposee core penetrates the channel.
Such a pathological state of vertebrates predisposes to compression of the spinal cord and the development of discogenic myelopathy.Clinically, it manifests itself in Torpor, the weaknesses of some muscle groups of the legs or arms, paresis, muscle atrophy, a change in tendon reflexes.Disorders of emptying the bladder and (or) intestines may also be observed.As a result of the formation of intervertebral hernia, arteries that feed the spinal cord are squeezed.Ischemic areas are formed, in which all nerve cells were killed.The so -called neurological deficit occurs - movements are violated, sensitivity is reduced, and trothy is upset.

Tactics of treatment
Osteochondrosis does not lend itself to complete cure, as so far drugs have not yet been synthesized, the intake of which would help restore damaged intervertebral discs and vertebrae.But the therapeutic schemes necessarily include Chondroprotectors - symptomatic agents of a slow action.Preference is given to drugs with active chondroitin ingredients with sulfate and (or) glucosamine sulfate (hydrochloride).
The clinical effectiveness of these drugs is confirmed by the results of many years of research.With prolonged admission (from 3 months to 2 years), partial regeneration of cartilaginous tissues occurs, as well as other connective tissue structures - ligaments, tendons, bournes.As they accumulate in the intervertebral discs of glucosamine and chondroitin, they begin to exert a pronounced analgesic, decongestant, anti -inflammatory effect.This allows you to reduce the doses of NSAIDs, glucocorticosteroids, muscle relaxants, thereby reducing the pharmacological load on the body.
Drugs for joints are ineffective with irregular use or their use for the treatment of osteochondrosis of the 3rd degree, when significant destruction of cartilage tissues is observed.
To eliminate symptoms that usually occur with cervical or breast osteochondrosis, drugs are used to improve blood circulation, nootropics, a drug that improves the microcirculation of the labyrinth used for the pathology of the vestibular apparatus.
If necessary, antidepressants, anticonvulsants are included in therapeutic schemes.
In the treatment of osteochondrosis, physiotherapeutic procedures are used: UHF therapy, magnetotherapy, laser therapy.Reflexotherapy, massage, exercise therapy, hirudotherapy, swimming, yoga are used.With the ineffectiveness of conservative treatment, the patient is shown surgical intervention.Practices are practiced by the disk, its laser reconstruction or replacement of the implant.
































